Ultra–hygienic and strict standards of sterilization are maintained.
Sterilization in dental practices is crucial to prevent cross-contamination and ensure the safety of both patients and dental professionals. The sterilization process involves several steps, including cleaning, disinfecting, and sterilizing instruments and equipment. Here is an overview of the sterilization process in a dental context:
1. Cleaning
Manual Cleaning:
Rinsing: Instruments should be rinsed under running water to remove any visible debris.
Scrubbing: Use brushes to scrub instruments manually, paying attention to hinges and crevices.
Ultrasonic Cleaning:
Ultrasonic Bath: Instruments are placed in an ultrasonic cleaner filled with a cleaning solution. The ultrasonic waves create tiny bubbles that help remove debris from instruments.
2. Disinfection
Surface Disinfection:
Wipes/Sprays: Use EPA-approved disinfectant wipes or sprays to clean surfaces, dental chairs, and countertops.
Drying: Allow surfaces to air dry or use a clean towel to wipe them down.
3. Packaging
Instrument Packs: After cleaning, instruments should be dried and then placed in sterilization pouches or wraps. The packaging should be permeable to the sterilization agent (steam, chemical vapor, or dry heat) but should maintain sterility after the process.
4. Sterilization Methods
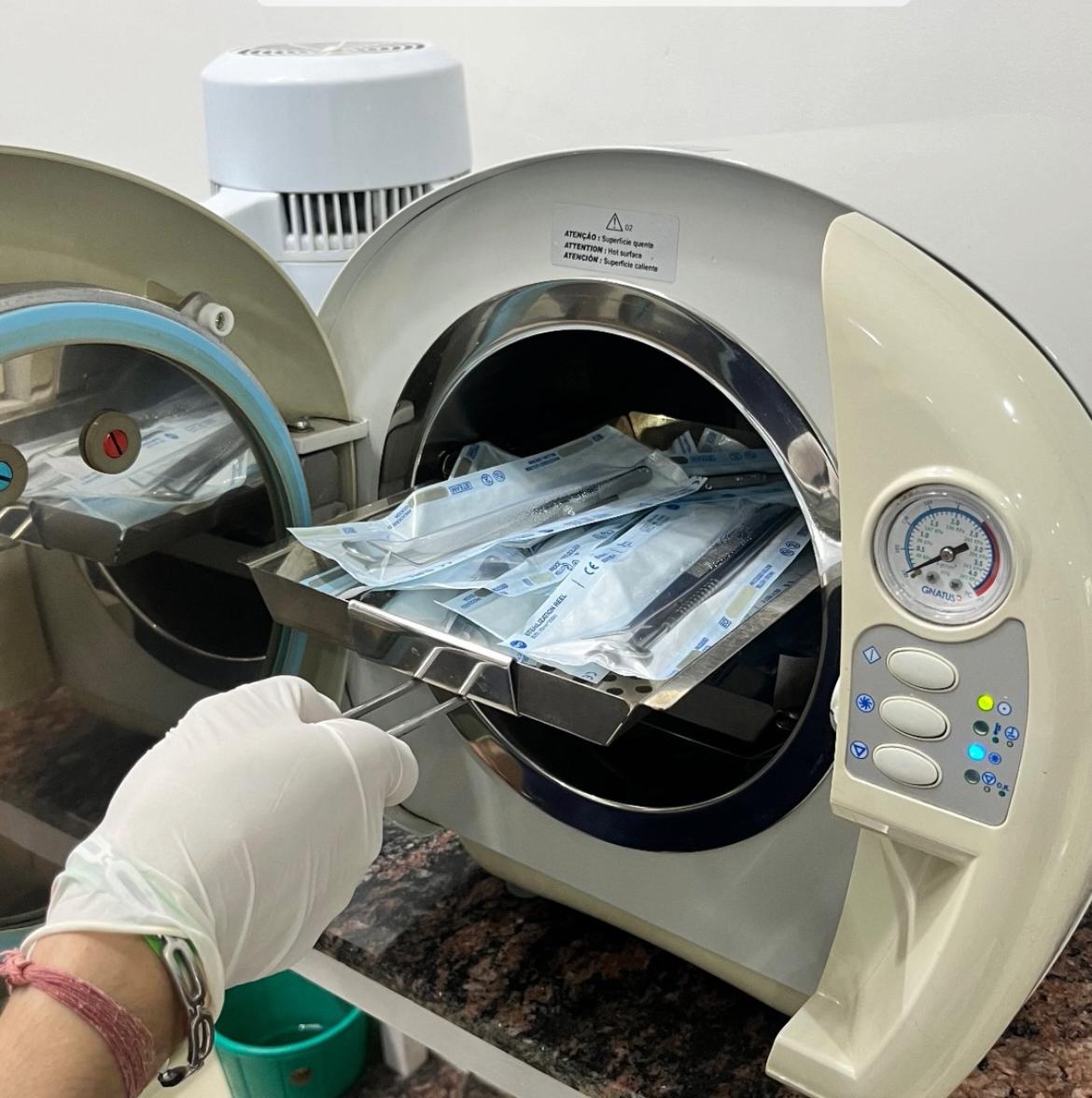
Steam Sterilization (Autoclaving):
Autoclaves: Use pressurized steam at high temperatures (121°C to 134°C) for specific time intervals to kill all microorganisms.
Cycle: Typical cycles involve a heating phase, sterilization phase, and drying phase.
Chemical Vapor Sterilization:
Chemiclaves: Use a mixture of chemicals, such as alcohol, formaldehyde, and other agents, heated under pressure to achieve sterilization.
Advantages: Faster cycle times and less corrosive to instruments than steam.
Dry Heat Sterilization:
Ovens: Use high temperatures (160°C to 190°C) for extended periods to sterilize instruments.
Non-Corrosive: Suitable for instruments that might be damaged by moisture.
5. Storage
Sterile Storage: Store sterilized instruments in a clean, dry, and closed environment to maintain sterility until use.
6. Monitoring
Biological Indicators:
Spore Tests: Use biological indicators containing spores of heat-resistant bacteria to verify the efficacy of the sterilization process.
Chemical Indicators:
Indicator Strips: Place chemical indicator strips inside packaging to ensure that the sterilizing agent has penetrated the pack.
Mechanical Indicators:
Cycle Logs: Autoclaves and other sterilizers often have printouts or digital logs that record the parameters of each cycle, such as temperature, pressure, and time.
7. Documentation
Record Keeping: Maintain records of sterilization cycles, including biological and chemical indicator results, to ensure compliance with regulatory standards.
Key Considerations
Infection Control Protocols:
Establish and follow infection control protocols as recommended by organizations such as the Centers for Disease Control and Prevention (CDC) and the American Dental Association (ADA).
Training:
Regularly train and update dental staff on proper sterilization techniques and protocols to ensure consistency and safety.
Equipment Maintenance:
Regularly inspect and maintain sterilization equipment to ensure it operates efficiently and effectively.
Cleaning and Disinfecting the Examining Room
Between each patient, the treatment rooms are thoroughly cleaned and disinfected. After a thorough clean up, a disinfectant is sprayed on all surfaces.
Sterilization of Dental Instruments
Needles used for local anesthesia are single use & disposable. The reusable instruments are cleaned treated with special sterilizing liquids. Then, they are packaged and heat sterilized in a large, pressurized oven – Autoclave. This ensures complete freedom from all bacteria, viruses and even spores (which are tougher microorganisms that resist simple cleaning procedures). We test our sterilization units frequently to make sure that they are working properly.
Please feel free to contact our office if you have any further questions or concerns.